Introduction
In recent years, scientific research has revealed a remarkable connection between two seemingly unrelated areas of our body: mitochondria, known as the "powerhouses of the cell," and the gut microbiome, a complex ecosystem of microorganisms inhabiting our intestines. This connection has far-reaching implications for our overall health and well-being. In this article, we will delve into the fascinating world of cellular biology and microbiology to explore how mitochondria and the gut microbiome jointly influence our health and how we can optimize this symbiosis.
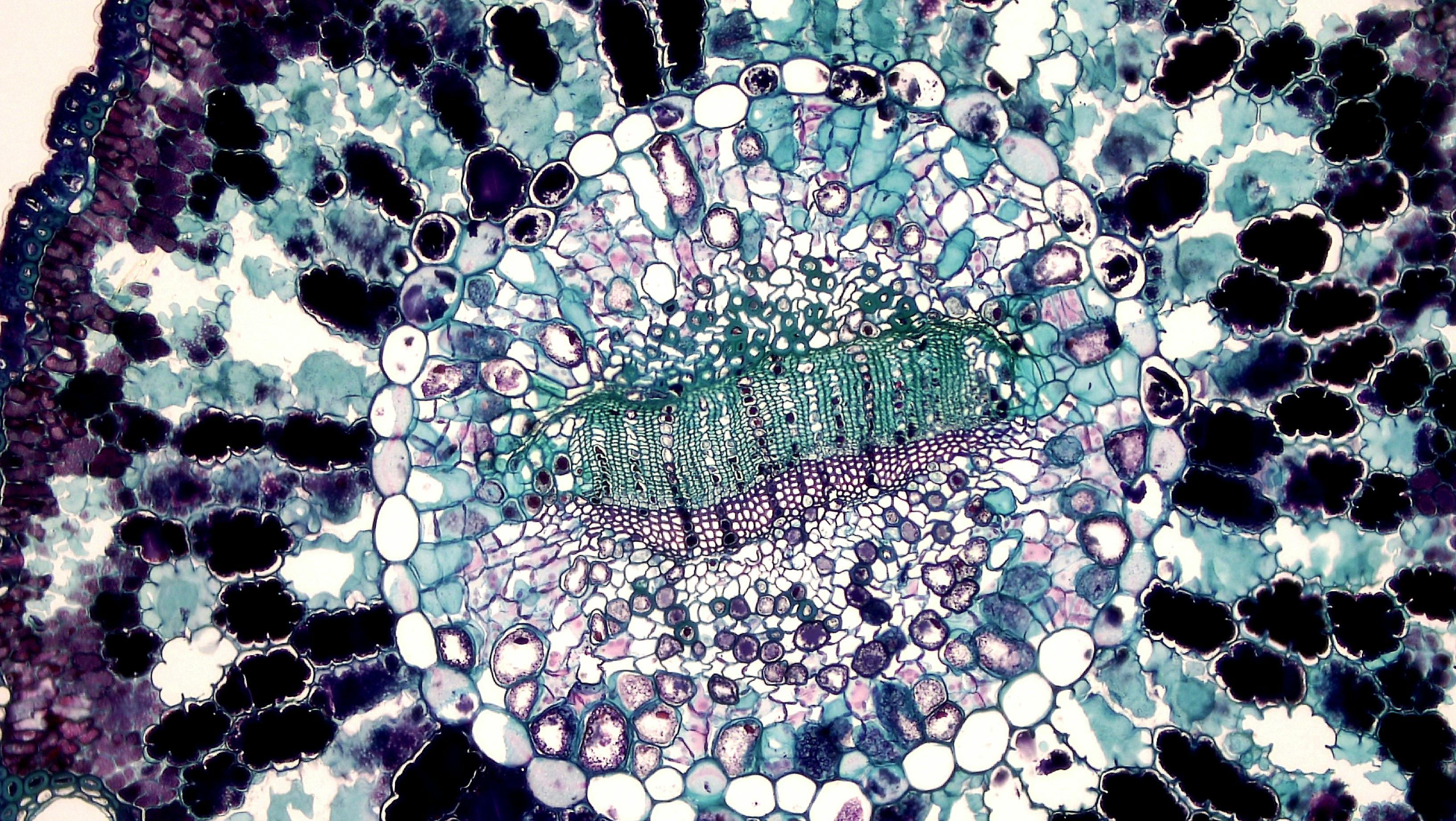
Mitochondria as the control center of cellular signaling
Mitochondrial colonies in our cells function as the main generator of ROS/RNS signals (reactive oxygen and nitrogen species), and thus also bio-photon emissions. These signals play a key role in cellular communication and metabolism [1].
These signals are further influenced and finely tuned by quantum communication through water networks and cell membranes. Research suggests that this quantum communication may be crucial for synchronizing cellular functions and may affect the overall homeostasis of the organism [2].
Role of Melanin in the Regulation of Cellular Signals
Melanin, a pigment known primarily for its role in skin and hair color, actually has a much broader biological significance. It absorbs excess biophotons or ROS/RNS signals, thereby controlling the timing of our cells and inflammatory signals in any cell where POMC (pro-opiomelanocortin) is expressed [3].
Interestingly, gut microbes emit 5000 times more light than our human cells [4]. These light signals must be properly regulated in a quantum manner through quorum sensing and quantum coherence. This process allows bacteria to communicate and coordinate their behavior, which has a crucial impact on the function of the gut microbiome [5].
Alfa-MSH: A Key Player in Gut Health
Alfa-MSH (alpha-melanocyte stimulating hormone) acts as a precursor for melanin production. It has a significant impact on cytokines in the intestines and exhibits antimicrobial properties against various pathogens [6].
Studies have shown that alpha-MSH can reduce inflammation in the intestines and support the integrity of the intestinal barrier. These effects may be especially important in the treatment of inflammatory bowel diseases such as Crohn's disease or ulcerative colitis [7].
The Impact of Sunlight on the Gut Microbiome
Sunlight surprisingly has a significant impact on our gut health. It increases the production of α-MSH/melanin, vitamin D, dopamine, serotonin, and nitric oxide, all of which affect the enteric nervous system [8].
The sunlight itself also modulates the composition of the gut microbiome. Studies on mice have shown that exposure to UV radiation can change the diversity of gut bacteria and potentially improve gut health [9].
It is important to realize that dietary supplements in the modern world are only a poor substitute for molecules obtained from sunlight. Natural exposure to sunlight can have more complex and beneficial effects on our body than isolated supplements [10].
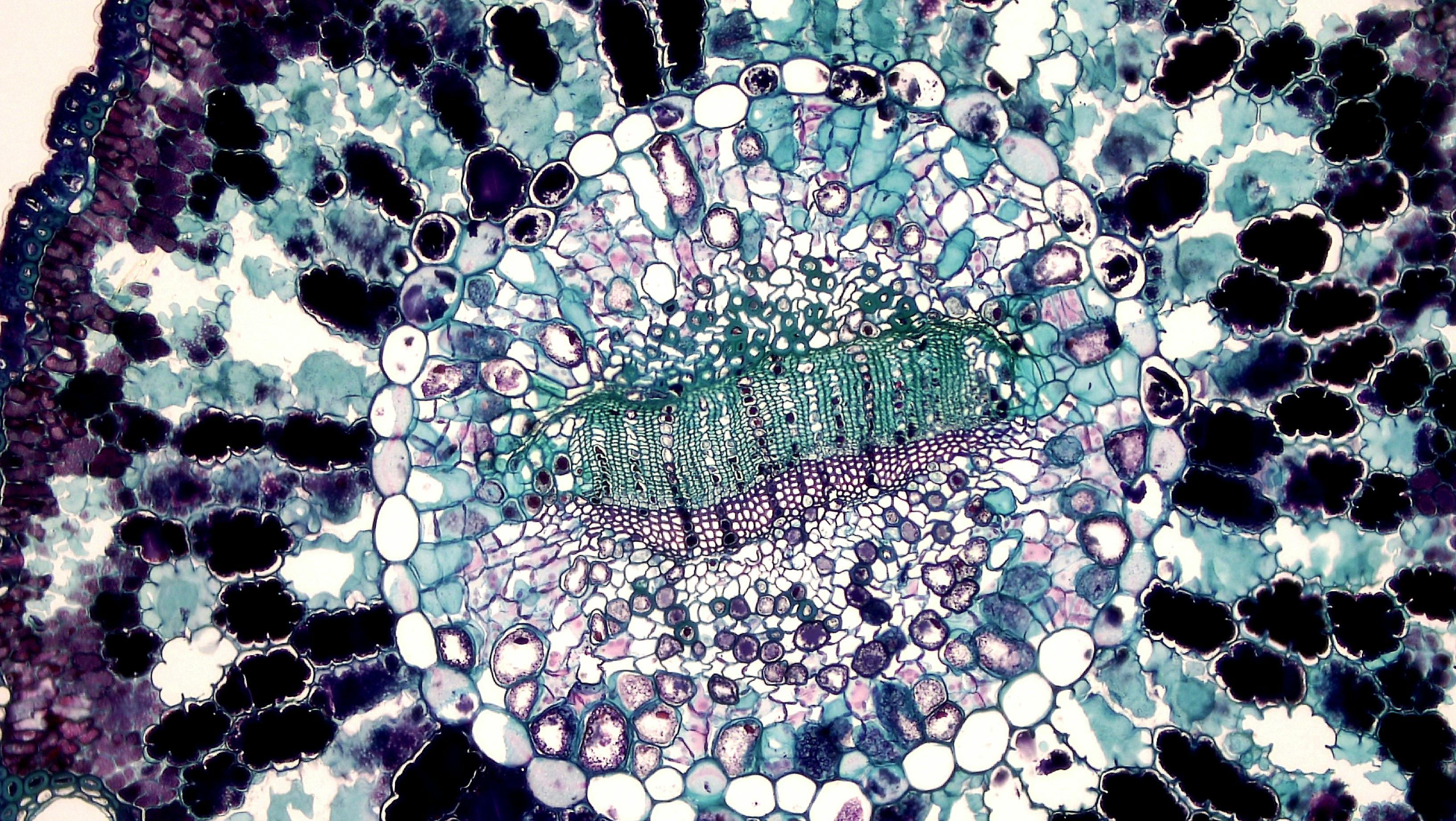
Cytokines and Cellular Communication
Cytokines are small proteins that play a key role in cellular signaling. They act as signals altering biophoton emissions and ROS/RNS signals within cells, thereby influencing communication between cells and between cells and the microbiome [11].
This complex communication network subsequently affects a number of physiological processes, including:
- Intestinal permeability
- Nutrient absorption
- Function of the vagus nerve
- Function of enteroendocrine cells
- Axes hypothalamus-pituitary-adrenal
- Intestinal lymphoid tissues (GALT)
Disruptions in this communication can lead to various health problems, ranging from inflammatory bowel diseases to systemic inflammations and autoimmune disorders [12].
Mitochondrial Redox State and Gut Microbiome
The redox state of mitochondria plays a key role in cellular metabolism and influences the composition of the gut microbiome. This state balances oxidized/reduced/other molecules, including:
- ROS/RNS
- ATP
- NAD+/NADH
- NADP+/NADPH
- mtDNA
- Intermediates of the Krebs cycle
- Various other metabolites
All these factors directly and indirectly affect the composition of the gut microbiome [13]. For example, changes in the NAD+/NADH ratio can influence the metabolism of gut bacteria and thus their growth and reproduction [14].
Mitochondrial Dysfunction and Its Impacts
Mitochondrial dysfunction can have serious consequences for gut health. It leads to the accumulation of molecular oxygen (O2) in the intestinal lumen, which promotes the production of pathogenic bacteria and disrupts efficient bioenergetics throughout the gut [15].
This dysfunction also impairs the synthesis of short-chain fatty acids, such as butyrate. Butyrate is key to the health of intestinal cells and has anti-inflammatory effects [16].
Mitochondrial dysfunction in enterocytes (intestinal cells) also leads to disruption of the intestinal lining, resulting in a permeable intestinal barrier and blood-brain barrier. This condition, known as "leaky gut," is associated with a range of health issues, from allergies to autoimmune diseases [17].
Symptoms of Intestinal Problems as an Indicator of Mitochondrial Dysfunction
When symptoms such as flatulence, bloating, constipation, diarrhea, heartburn, etc. appear, it is often a sign of mitochondrial/bioenergetic problems in the affected area of the intestines. These symptoms should not be underestimated, as they may indicate deeper issues in cellular metabolism [18].
Natural Ways to Optimize Mitochondrial Function
There are several natural ways to support mitochondrial health and thus the gut microbiome:
1. Infrared light: Exposure to infrared light can stimulate mitochondrial function and support cellular energy [19].
2. Grounding: Contact with the earth (so-called "earthing") can help reduce oxidative stress and inflammation in the body [20].
3. Reducing stress and toxins: Chronic stress and exposure to toxins can damage mitochondria. Minimizing these factors is crucial for mitochondrial health [21].
4. Optimized diet: A nutrient-rich diet, especially one aligned with natural light cycles (seasonal foods), can significantly support mitochondrial function [22].
Conclusion
The connection between mitochondria and the gut microbiome represents a fascinating area of research with potentially far-reaching implications for human health. Understanding this complex interaction allows us to better comprehend how our body functions at the cellular level and how we can optimize our health.
The key insight is that our body is deeply connected with natural rhythms and processes. From sunlight to seasonal foods, returning to natural ways of living can significantly support the health of our mitochondria and gut microbiome.
Future research in this area promises new insights into the prevention and treatment of various diseases, from metabolic disorders to neuropsychiatric conditions. In the meantime, we can use current knowledge to optimize our lifestyle and support health at the cellular level.
Remember that the path to health begins with the smallest components of our body - our cells and the microorganisms that live with us in symbiosis. Let's take care of them, and they will take care of us.
Reference
[1] Murphy, M. P. (2009). How mitochondria produce reactive oxygen species. Biochemical Journal, 417(1), 1-13. [https://doi.org/10.1042/BJ20081386](https://doi.org/10.1042/BJ20081386)
[2] Pokorný, J., Vedruccio, C., Cifra, M., & Kučera, O. (2011). Cancer physics: diagnostics based on damped cellular elastoelectrical vibrations in microtubules. European Biophysics Journal, 40(6), 747-759. [https://doi.org/10.1007/s00249-011-0697-0](https://doi.org/10.1007/s00249-011-0697-0)
[3] Slominski, A., Tobin, D. J., Shibahara, S., & Wortsman, J. (2004). Melanin pigmentation in mammalian skin and its hormonal regulation. Physiological Reviews, 84(4), 1155-1228. [https://doi.org/10.1152/physrev.00044.2003](https://doi.org/10.1152/physrev.00044.2003)
[4] Thar, R., & Kühl, M. (2004). Propagation of electromagnetic radiation in mitochondria?. Journal of Theoretical Biology, 230(2), 261-270. [https://doi.org/10.1016/j.jtbi.2004.05.021](https://doi.org/10.1016/j.jtbi.2004.05.021)
[5] Miller, M. B., & Bassler, B. L. (2001). Quorum sensing in bacteria. Annual Reviews in Microbiology, 55(1), 165-199. [https://doi.org/10.1146/annurev.micro.55.1.165](https://doi.org/10.1146/annurev.micro.55.1.165)
[6] Catania, A., Gatti, S., Colombo, G., & Lipton, J. M. (2004). Targeting melanocortin receptors as a novel strategy to control inflammation. Pharmacological Reviews, 56(1), 1-29. [https://doi.org/10.1124/pr.56.1.1](https://doi.org/10.1124/pr.56.1.1)
[7] Brzoska, T., Luger, T. A., Maaser, C., Abels, C., & Böhm, M. (2008). Alpha-melanocyte-stimulating hormone and related tripeptides: biochemistry, antiinflammatory and protective effects in vitro and in vivo, and future perspectives for the treatment of immune-mediated inflammatory diseases. Endocrine Reviews, 29(5), 581-602. [https://doi.org/10.1210/er.2007-0027](https://doi.org/10.1210/er.2007-0027)
[8] Feelisch, M., Kolb-Bachofen, V., Liu, D., Lundberg, J. O., Revelo, L. P., Suschek, C. V., & Weller, R. B. (2010). Is sunlight good for our heart?. European Heart Journal, 31(9), 1041-1045. [https://doi.org/10.1093/eurheartj/ehq069](https://doi.org/10.1093/eurheartj/ehq069)
[9] Wang, J., Wang, Y., Gao, W., Wang, B., Zhao, H., Zeng, Y., ... & Zhao, L. (2017). Diversity analysis of gut microbiota in osteoporosis and osteopenia patients. PeerJ, 5, e3450. [https://doi.org/10.7717/peerj.3450](https://doi.org/10.7717/peerj.3450)
[10] Holick, M. F. (2004). Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. The American Journal of Clinical Nutrition, 80(6), 1678S-1688S. [https://doi.org/10.1093/ajcn/80.6.1678S](https://doi.org/10.1093/ajcn/80.6.1678S)
[11] Zhang, J. M., & An, J. (2007). Cytokines, inflammation and pain. International Anesthesiology Clinics, 45(2), 27. [https://doi.org/10.1097/AIA.0b013e318034194e](https://doi.org/10.1097/AIA.0b013e318034194e)
[12] Schoultz, I., & Keita, Å. V. (2020). The intestinal barrier and current techniques for the assessment of gut permeability. Cells, 9(8), 1909. [https://doi.org/10.3390/cells9081909](https://doi.org/10.3390/cells9081909)
[13] Saint-Georges-Chaumet, Y., & Edeas, M. (2016). Microbiota–mitochondria inter-talk: consequence for microbiota–host interaction. Pathogens and Disease, 74(1), ftv096. [https://doi.org/10.1093/femspd/ftv096](https://doi.org/10.1093/femspd/ftv096)
[14] Belenky, P., Bogan, K. L., & Brenner, C. (2007). NAD+ metabolism in health and disease. Trends in Biochemical Sciences, 32(1), 12-19. [https://doi.org/10.1016/j.tibs.2006.11.006](https://doi.org/10.1016/j.tibs.2006.11.006)
[15] Bratic, A., & Larsson, N. G. (2013). The role of mitochondria in aging. The Journal of Clinical Investigation, 123(3), 951-957. [https://doi.org/10.1172/JCI64125](https://doi.org/10.1172/JCI64125)
[16] Hamer, H. M., Jonkers, D. M. A. E., Venema, K., Vanhoutvin, S. A. L. W., Troost, F. J., & Brummer, R. J. (2008). Review article: the role of butyrate on colonic function. Alimentary Pharmacology & Therapeutics, 27(2), 104-119. [https://doi.org/10.1111/j.1365-2036.2007.03562.x](https://doi.org/10.1111/j.1365-2036.2007.03562.x)
[17] Mu, Q., Kirby, J., Reilly, C. M., & Luo, X. M. (2017). Leaky gut as a danger signal for autoimmune diseases. Frontiers in Immunology, 8, 598. [https://doi.org/10.3389/fimmu.2017.00598](https://doi.org/10.3389/fimmu.2017.00598)
[18] Naviaux, R. K. (2014). Metabolic features of the cell danger response. Mitochondrion, 16, 7-17. [https://doi.org/10.1016/j.mito.2013.08.006](https://doi.org/10.1016/j.mito.2013.08.006)
[19] Hamblin, M. R. (2016). Shining light on the head: photobiomodulation for brain disorders. BBA Clinical, 6, 113-124. [https://doi.org/10.1016/j.bbacli.2016.09.002](https://doi.org/10.1016/j.bbacli.2016.09.002)
[20] Chevalier, G., Sinatra, S. T., Oschman, J. L., Sokal, K., & Sokal, P. (2012). Earthing: health implications of reconnecting the human body to the Earth's surface electrons. Journal of Environmental and Public Health, 2012. [https://doi.org/10.1155/2012/291541](https://doi.org/10.1155/2012/291541)
[21] Picard, M., McEwen, B. S., Epel, E. S., & Sandi, C. (2018). An energetic view of stress: Focus on mitochondria. Frontiers in Neuroendocrinology, 49, 72-85. [https://doi.org/10.1016/j.yfrne.2018.01.001](https://doi.org/10.1016/j.yfrne.2018.01.001)
[22] Kuo, Y. T., Shih, P. H., Kao, S. H., Yeh, G. C., & Lee, H. M. (2015). Pyrroloquinoline quinone resists denervation-induced skeletal muscle atrophy by activating PGC-1α and integrating mitochondrial electron transport chain complexes. PLoS One, 10(12), e0143600. [https://doi.org/10.1371/journal.pone.0143600](https://doi.org/10.1371/journal.pone.0143600)

Leave a comment
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.